One of the things I’ve noticed as an American gynecologist practicing in Paris is that all excisional procedures of the cervix are lumped together into one word in France: Conisation!
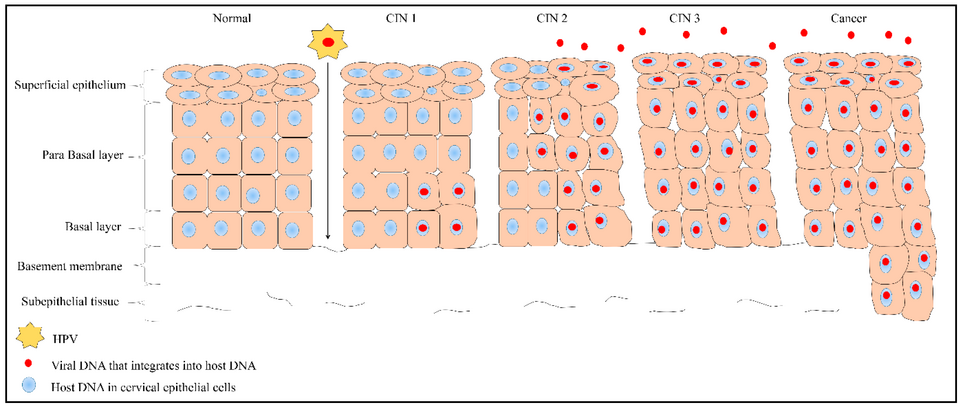
You may have heard this word if your frottis (HPV test or pap smear) is abnormal and then you undergo a colposcopy. If the biopsies taken during a colposcopy reveal a high-grade lesion (CIN2, CIN3, AIS), your gynecologist probably recommended a conisation. At this point you’re probably alarmed, since you are dealing with a pre-cancerous lesion of the cervix. But on top of that, as an expat in Paris, you may be left wondering, what is a conisation exactly? Terminology changes across different countries, but also surgical techniques, and that matters, since not all conisations are the same! So as The Bard said, “What’s in Name?” In this case, a lot.
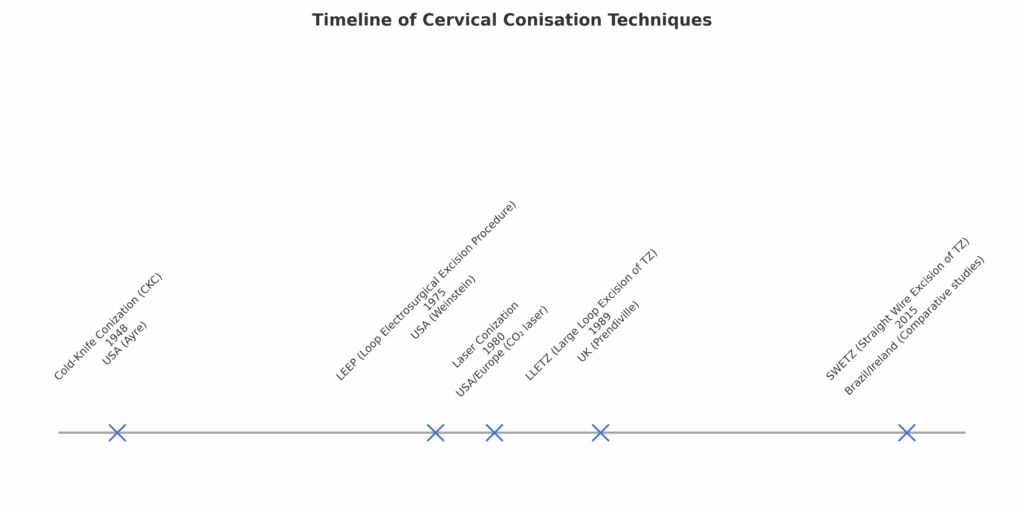
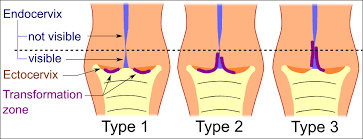
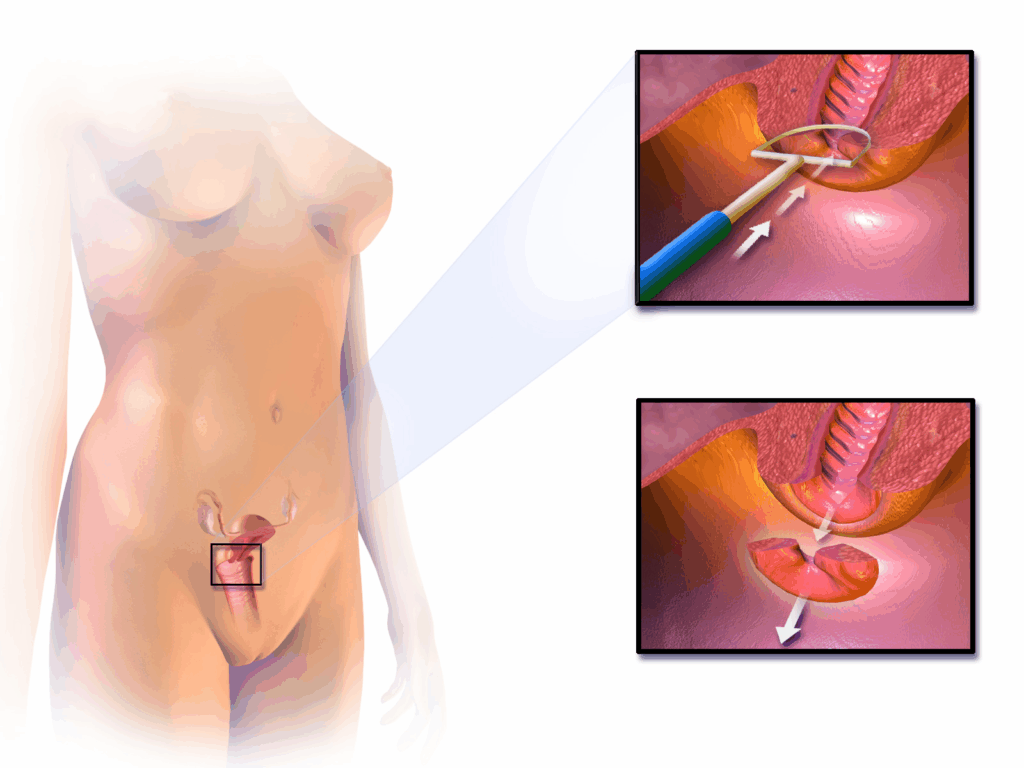
I know how stressful it can be to face an abnormal result a foreign healthcare system — especially when the terminology is unfamiliar. This guide will explain the differences between the various techniques (LEEP, LLETZ, CKC, or SWETZ), what each one means for your health and fertility, and how to ask the right questions so that you feel empowered in your care.
The procedure coding system in France (CCAM), calls all of these Conisation du col de l’uterus in French, so which one should you get?!
If you are not considering carrying a pregnancy in the future, you can skip this section.
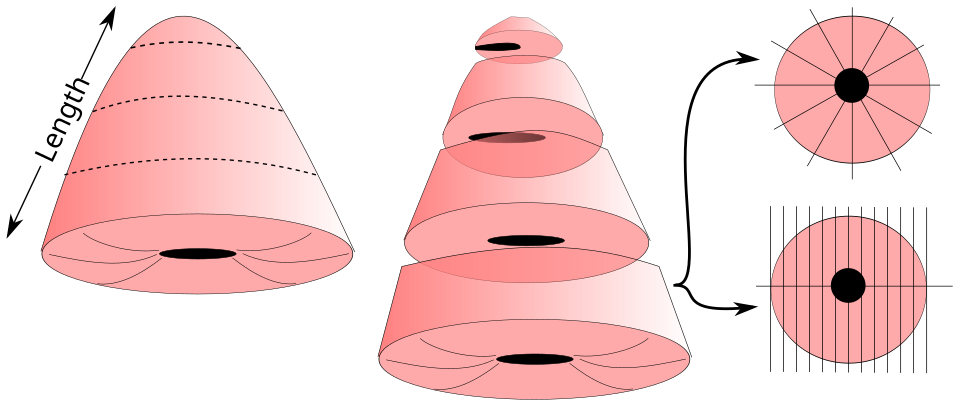
If you are, you may know that one of the most feared complications from any cervical tissue excision is increased risk of preterm birth (PTB) in future pregnancies. This is because shortening the cervix (by removing portions of it), from a baseline of ~4 cm, to let’s say 2 cm, can affect the integrity of the cervical tissue and its ability to stay closed during pregnancy. While the cervix should eventually open (dilate) in order to allow for a vaginal birth, when it opens prior to 37 weeks, we call it pre-term labor, which of course can come with complications for your baby. However, the relationship between LEEPs and PTB is not so clear, and you should NOT be afraid to get a LEEP. Here’s why:
Association vs causation; confounding by indication
Larger excisions / deeper cones correlate with higher risk
Don’t be afraid of a small LEEP
If you are currently pregnant
It is normal to be anxious when facing cervical surgery, especially if you hope to have children in the future and don’t understand the terminology in French. The good news is that modern approaches emphasize tailored, conservative treatment. In the majority of cases, a LEEP removes all abnormal cells while preserving healthy cervical tissue. Asking your gynecologist about their surgical approach, excision depth, and use of colposcopy ensures that you remain in control of your health decisions. From a patient’s perspective, it’s quite reasonable to ask your surgeon:
If you live in Paris as an expat and are told you need a conisation, remember: not all conisations are the same. For most patients, a simple LEEP is safe, effective, and fertility-preserving. Glandular lesions may require a deeper cone, but even then, careful technique helps minimize risks. Always discuss the surgical approach with your gynecologist to ensure the best balance between cure and future pregnancy outcomes.
Understanding Adenomyosis: A Guide for English-Speaking Expats Living in Paris For many English-speaking expats living in Paris, it can be challenging to navigate a different
Understanding Uterine Fibroids: What You Need to Know Uterine fibroids, also known as leiomyomas or myomas, are noncancerous growths that develop in or around the
American Hospital of Paris
55 Boulevard du Château,
92200 Neuilly-sur-Seine
+33 (0) 1 46 41 26 99
2025 © Dr Ramírez Zamudio