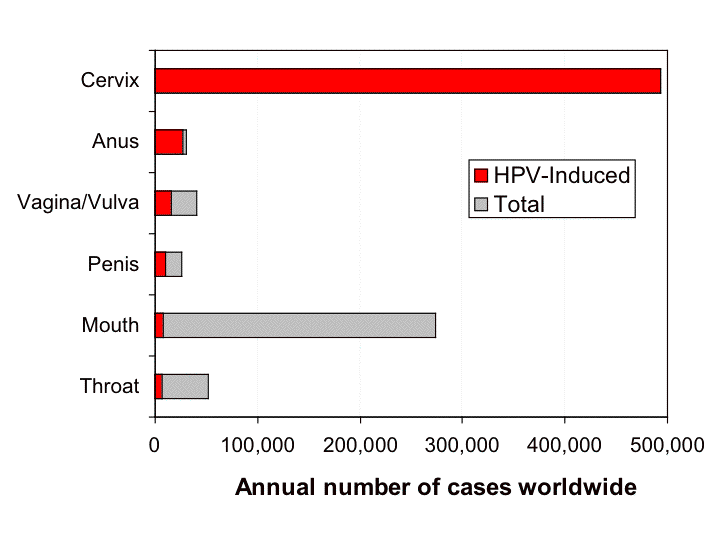
Human Papilloma Virus (HPV) affects up to 80% of people during their lifetime and can impact various areas of the body including the cervix, vagina, vulva, anus, penis, and throat.
While many HPV infections resolve on their own, persistent infection can lead to dysplasia—a change in the cells that may become cancerous if untreated. Thankfully, this process is slow, often taking over a decade, and there are many opportunities to screen, monitor, and treat HPV-related changes before they become dangerous.
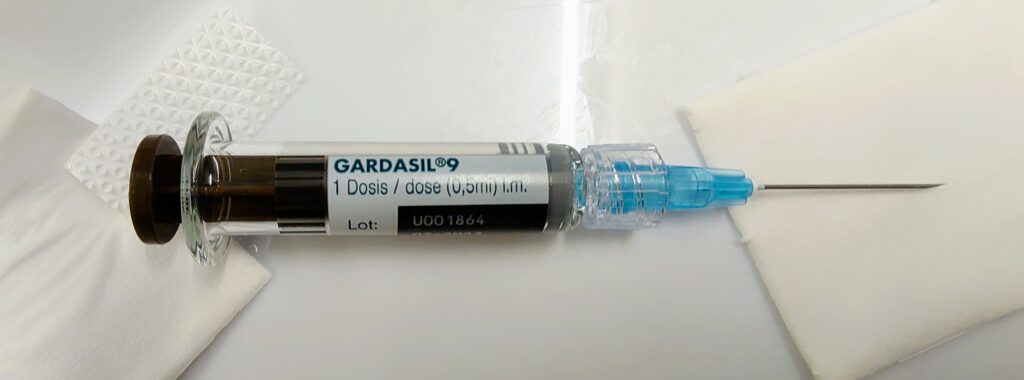
In the United States, the HPV vaccine is routinely offered starting at age 11 or 12 to girls and boys. Because we may not all have had the vaccine during adolescence (often when parents make decisions for us), catch-up vaccinations is available up to age 26, and in some cases up to age 45. The vaccine protects against 9 strains of HPV that are responsible for cervical, anal, vulvar, and throat cancers—as well as genital warts. Even if you have been affected by one strain of HPV already, the vaccine may still be beneficial in protecting you against the eight other strains it contains, so I often recommend it even for adults that are already sexually active.
In France, vaccination is recommended starting at age 11 for boys and girls, and as of 2023, they started a voluntary school-based vaccination program for middle school students around age 12. Catch-up vaccination to age 26 was previously only offered to Men who have Sex with Men (MSM), but as of May 16, 2025, it is (finally!) available for all women and men, regardless of sexual practices, up to age 26. However, many expat women and men may have missed the window due to living abroad during adolescence, and still wonder if the vaccine is worthwhile. The answer is often YES, and a consultation can help you assess whether it’s recommended based on your history.
Another common question is whether boys can benefit as much as girls from the vaccination. The answer again is a resounding YES!, since the vaccine also protects against penile, anal and throat cancers. This is even without considering the obvious benefit of decreased transmission to sexual partners.
Because insurance coverage often lags after guidelines publication, the national healthcare program, Assurance Maladie, may not reimburse you for the vaccine up to age 26 yet, but you can always opt to pay for it out-of-pocket (it’s still a lot cheaper than in the U.S., and that treatments for HPV).
Though 90% of people will clear their initial HPV infection without any help, some will not and this will lead to persistent HPV infection. Persistent infection can lead to cellular changes called dysplasia or genital warts, and depending on the HPV strain, can even result in pre-cancerous lesions. If left untreated over time, these lesions are sadly the most common cause of cervical cancer. Dysplasia is usually detected through routine Pap smears or HPV tests, and confirmed by a colposcopy, a magnified exam of the cervix with acetic acid (vinegar) and possible biopsies.
There are different levels of dysplasia:
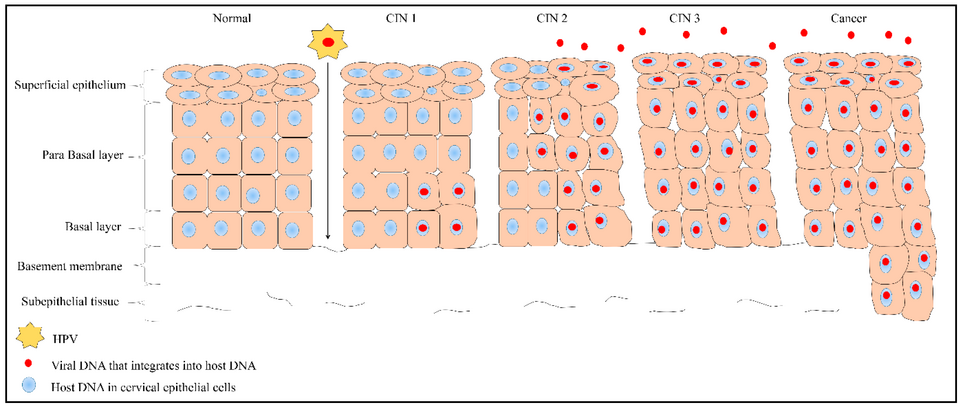
Thankfully high-grade lesions can be treated BEFORE they become cancerous, and the whole process from initial HPV infection to cancer takes around 10-15 years.
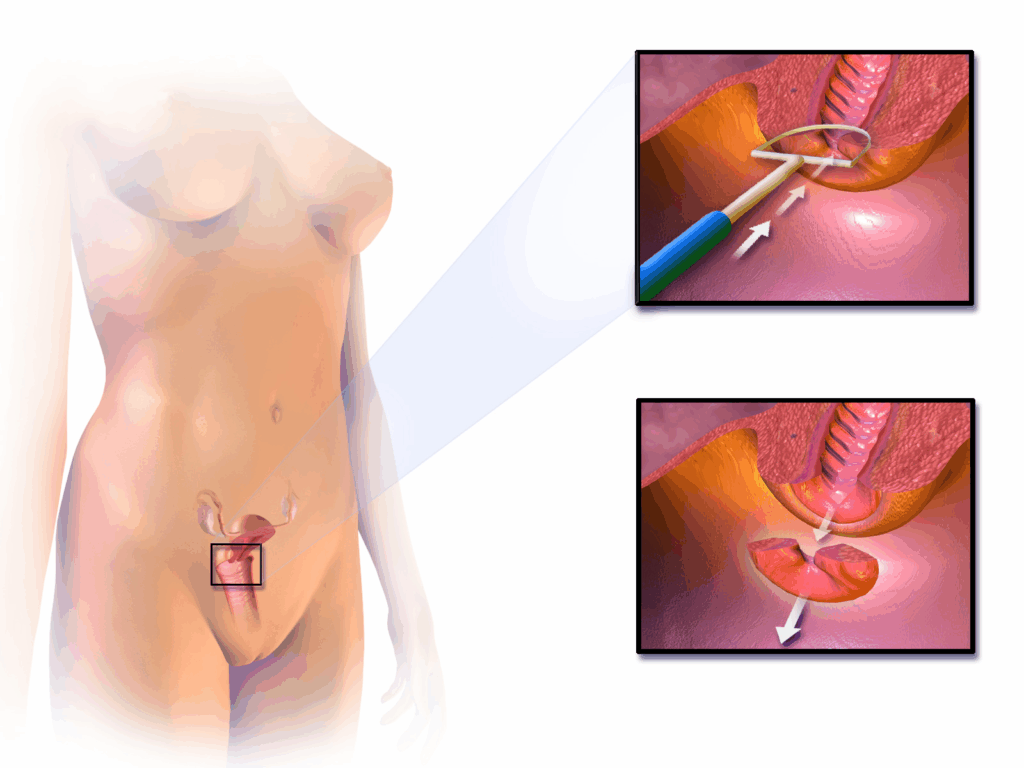
If you’ve been diagnosed with cervical dysplasia, treatment depends on the severity. Options include:
These procedures are often done in the office or outpatient setting, and are safe, effective, and fertility-preserving. In France, these procedures are often done in the operating room under general anesthesia. In the U.S., we often offer the option of LEEPs under local anesthesia, avoiding the need for ambulatory surgery. Because of my belief in patient-centered care, I offer both options based on patient preference and the extent of excision required.
While cervical dysplasia is most well-known, HPV can also cause anal dysplasia, vulvar dysplasia, and genital warts (condylomas). These conditions are more common in immunocompromised patients, people living with HIV, and men who have sex with men, but can occur in anyone. Like cervical changes, these lesions can be screened for and treated before they cause serious complications.
Treatment may include:
Successful HPV-related cancer prevention involves multiple strategies that include vaccination against HPV, protection with condoms, screening with HPV molecular tests (available for the cervix and anus) or “pap smears” of the cervix or anus, treatment of condylomas (warts) or precancerous lesions, and surveillance after treatment. These conditions are all preventable and treatable ! Whether you’re due for a Pap smear, have questions about the HPV vaccine, or need follow-up for an abnormal result, I’m available to guide you with clear communication, evidence-based care, and compassion.
The Importance of Anal Cancer Screening with HPV Molecular Testing Anal cancer is a rare but potentially deadly disease that has been increasing in prevalence
American Hospital of Paris
55 Boulevard du Château,
92200 Neuilly-sur-Seine
+33 (0) 1 46 41 26 99
2025 © Dr Ramírez Zamudio