For many English-speaking expats living in Paris, it can be challenging to navigate a different healthcare system while also trying to understand gynecologic conditions like adenomyosis and endometriosis. This article explains what adenomyosis is, how it relates to endometriosis, how it is diagnosed, and which treatment options are available—including medical treatments, uterine artery embolization, and hysterectomy using minimally invasive techniques.
Adenomyosis is a benign (non-cancerous) condition where tissue similar to the lining of the uterus (endometrium) grows inside the muscular wall of the uterus (the myometrium). Under the microscope, it is defined by endometrial glands and stroma located within the myometrium, often with thickening of the surrounding muscle.
Strictly speaking, adenomyosis is a histologic diagnosis—the gold standard has traditionally been examining the uterus after hysterectomy under the microscope.
However, we obviously do not remove most women’s uteri just to get a diagnosis! In daily practice, especially for women who wish to preserve fertility or their uterus, we rely on a combination of clinical symptoms such as heavy periods, painful periods, chronic pelvic pain, bloating, painful intercourse, and fertility issues, and imaging (transvaginal ultrasound and/or MRI).
So while “definitive” diagnosis is histological, most modern diagnoses are made based on imaging plus symptoms, using internationally accepted criteria.
Adenomyosis can be thought of as a subset of endometriosis since its underlying pathology stems from the same problem: endometrial tissue that migrates to a location is shouldn’t go to! In Endometriosis we often see these endometrial cells move from the inside of the uterus (endometrium) to parts outside the uterus such as the ovaries, pelvic peritoneum, bowel, bladder, and even more distant locations in the worst of cases. In Adenomyosis, these endometrial cells go into the uterine muscle (myometrium) and embed themselves there (see image below), causing localized inflammation, disruption the contractility of the myometrium and increasing its size many times.
When we understand that the underlying cause is the same, we understand why many treatment options also overlap.

There have been multiple prior attempts to implement a classification system for adenomyosis, but none have really taken off or correlated with clinical symptoms. However, for practical purposes, especially when considering surgical interventions, a simple classification can be helpful:
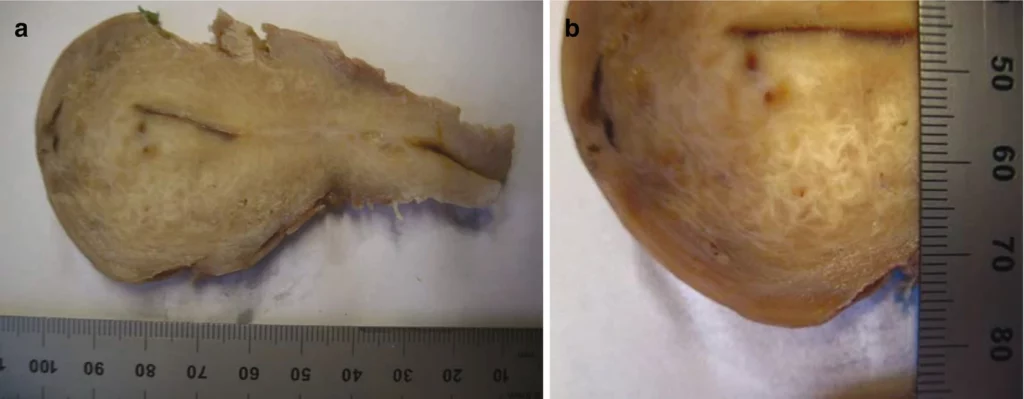
When adenomyosis is focal and forms a discrete mass-like lesion, this may be called an adenomyoma. An adenomyoma is essentially a nodular lump of adenomyosis: endometrial tissue embedded in a ball of thickened uterine muscle, and it can sometimes be mistaken for a fibroid on imaging.
These focal adenomyomas can cause heavy bleeding and pain—similar to diffuse adenomyosis—but sometimes lend themselves to more targeted surgical approaches such as removal or radiofrequency ablation of the mass with preservation of the uterus.
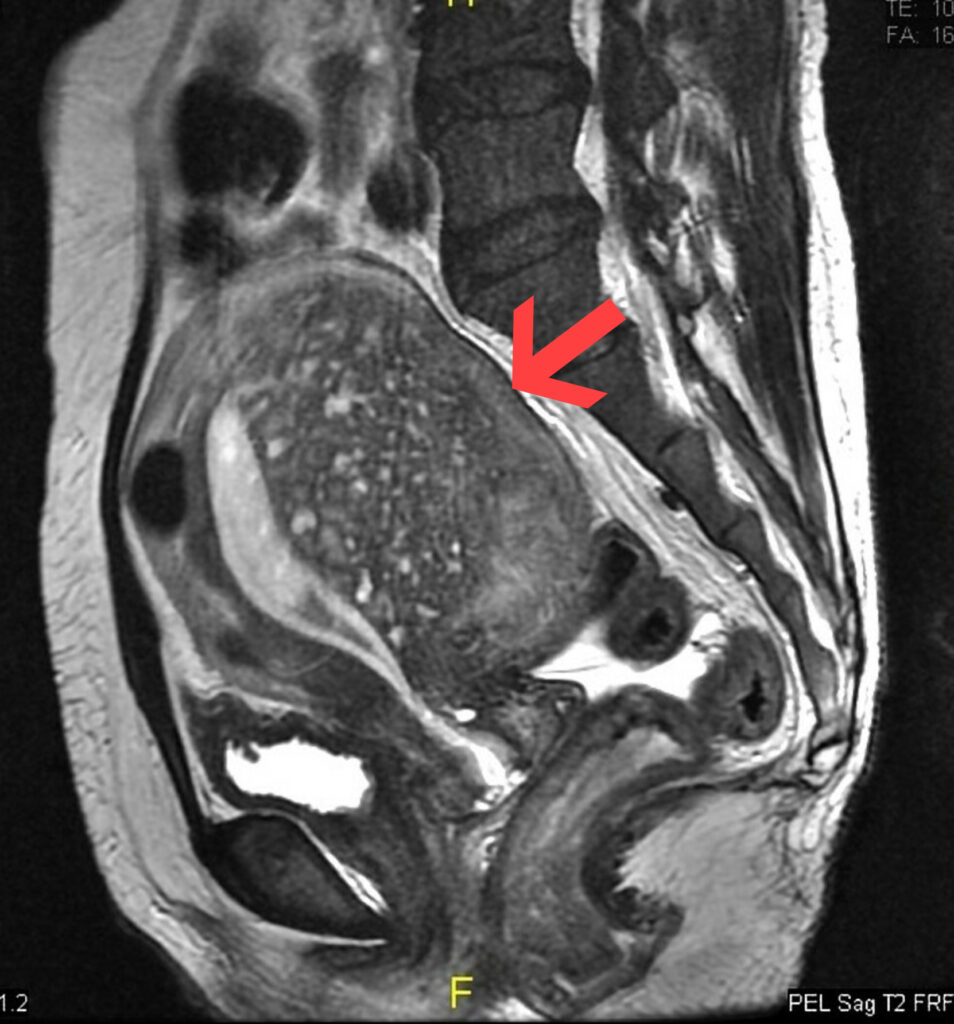
While transvaginal ultrasound is often the first test done in many countries, MRI is considered the best imaging modality for deeper forms of endometriosis and adenomyosis. Although studies comparing sensitivity and specificity (how good a test is at detecting a condition or not) between ultrasounds and MRIs have been mixed, the truth is that an ultrasound result depends on how good and experienced the sonographer is at detecting adenomyosis. MRI is a more objective test, and can better distinguish between soft tissues. Additionally, it examines the entire pelvis, so we can identify if there are areas of endometriosis (specially superficial implants) that are not easily seen on ultrasound.
The biggest drawback to MRI has historically been cost, which in places like the United States can be a couple of thousand dollars. Thankfully, this test in France is much more affordable and covered by insurance, whether it’s French social security or international insurance. Even without insurance, the out-of-pocket price for this test is around 250 euros. For many expats (and doctors like myself) used to the healthcare system in the United States, this is a pleasant surprise!
During perimenopause, hormone levels fluctuate and cycles can become irregular, heavy or prolonged.
If you already have underlying adenomyosis—even if it was silent before—these hormonal changes can unmask or worsen symptoms, particularly heavy bleeding and cramping. Many women present during this time with iron deficiency anemia caused by heavy bleeding, in addition to new onset pain that they thought was behind them. If this happens, make sure to seek consultation to obtain a diagnosis of why these new symptoms are happening and discuss possible treatment options.
Hormonal therapy with estrogens is often utilized to relieve symptoms of perimenopause and menopause, as well as to provide the medical benefits. However, estrogens can sometimes flare adenomyosis or unmask bleeding from adenomyosis, especially if the progestogen component of HT is not fully suppressing the lining. If you notice new or heavier bleeding on HRT, it is important to discuss with your gynecologist, possible obtain imaging to rule out adenomyosis, fibroids, polyps, or other pathology, and consider an alternative progestogen component, such as hormonal IUDs.
There is no single “best” treatment. The approach depends on:
In general, we start with medical management, then consider uterus-sparing procedures such as uterine artery embolization, and finally definitive surgery (hysterectomy) if symptoms remain severe.
How they work:
NSAIDs block prostaglandins, chemicals that cause uterine contractions and pain, reducing menstrual cramps and sometimes modestly reducing bleeding.
Effectiveness:
These medications can work very well for painful periods if taken correctly: ideally they should started 2 days before the onset of menses and continuing through the days of bleeding. However, for management of heavy bleeding due to adenomyosis, they are not as effective. They should be combined with another method.
Pros:
Cons:
How it works:
Tranexamic acid is an antifibrinolytic: it stabilizes blood clots in the endometrium so less blood is lost during menstruation.
Effectiveness:
Randomized controlled trials in patients who suffer from heavy menstrual bleeding (no matter the cause) have shown about a 34–40% reduction in menstrual blood loss compared with baseline and placebo. It is usually used for a maximum of 5 days per month, during the heaviest days of bleeding. However, TXA is not as effective as treating pain, so this can often be paired with NSAIDs (see above), to provide both pain relief and minimize bleeding.
Pros:
Cons:
Because adenomyosis is hormone-responsive, hormonal treatments aim to:
How it works:
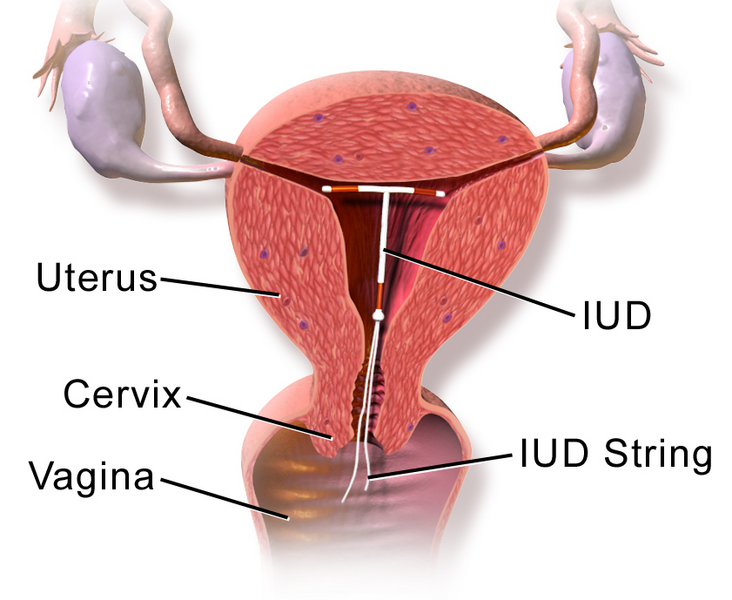
The device releases levonorgestrel directly into the uterine cavity, which:
Effectiveness:
Pros:
Cons:
How it works:
We call it the combined pill because it has both an estrogen and a progestin component. There are over 100 formulations of it based on type of estrogen, type of progestin, dose, number of days, etc, so it’s not a “one size fits all” type of medication and it may take time finding the right one for you. Of all the methods listed here, this is the only one that reliably suppresses ovulation and can be used in the long term (the other being GnRH agonists, see below).
Because it puts the ovaries “to sleep”, and the hormonal fluctuations due to ovulation don’t happen, it can also help with cases of ovarian cysts, PMS, or irregular bleeding. In the case of adenomyosis, it helps by thinning and stabilizing the endometrium, as well as endometrial tissue found elsewhere. The pill can also be taken continuously (without placebo) to reduce the number of withdrawal bleeds if we are trying to address anemia or heavy bleeding.
Effectiveness:
Data are stronger for endometriosis than adenomyosis, but many women see a 50–70% improvement in pain and bleeding, especially with continuous use.
Pros:
Cons:
How they work:
These pills are taken daily and only contain one type of hormone –progestins (as opposed to the combined pills discussed above). They work by:
Effectiveness:
Progestins such as dienogest are well studied in endometriosis and increasingly in adenomyosis, improving pain and bleeding scores and quality of life.
Pros:
Cons:
How it works:
Effectiveness:
French context – meningioma risk:
Pros:
Cons:
Despite these concerns, it remains an available and sometimes very useful option, particularly for women who prefer an injection every three months rather than daily tablets, after an informed discussion of risks and benefits.
How it works:
Effectiveness:
Pros:
Cons:
How they work:
Effectiveness:
Pros:
Cons:
What it is:
A minimally invasive radiologic procedure done by an interventional radiologist, traditionally used for fibroids but increasingly for adenomyosis.
How it works:
Effectiveness:
Pros:
Cons:
What it is:
Hysterectomy is removal of the uterus, sometimes with or without the cervix. The ovaries are preserved most of the time so hormonal function or status is not affected.
How it works:
Effectiveness:
Pros:
Cons:
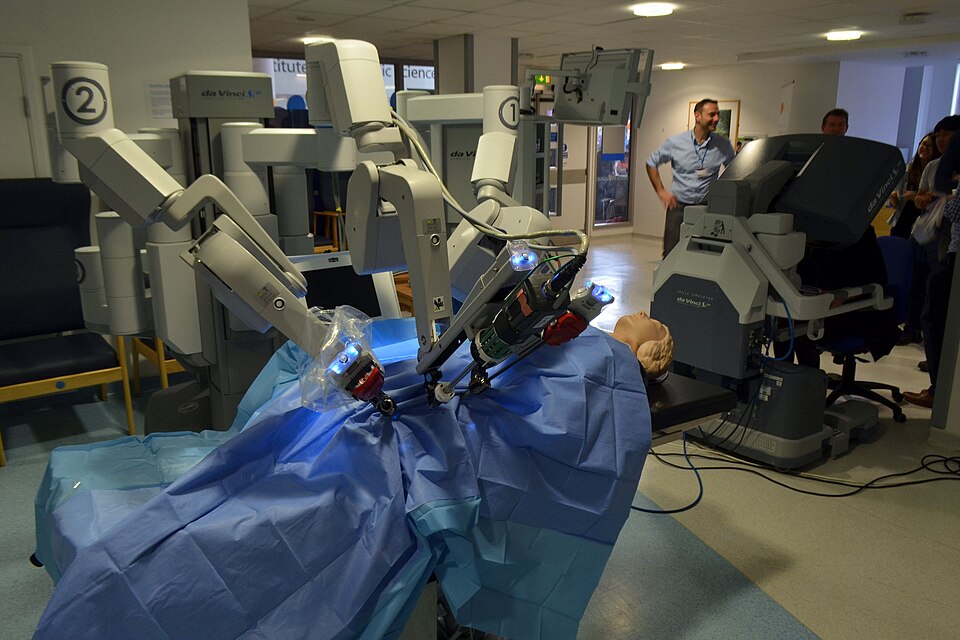
Whenever possible, hysterectomy should be performed using laparoscopic, robotic-assisted, or vaginal surgery techniques:
Advantages compared with open surgery:
In certain cases of focal adenomyomas, a uterus-sparing myometrial resection (adenomyomectomy) can also be considered via laparoscopy, especially in women seeking to preserve fertility, although this depends on lesion size, location, and overall uterine integrity.
For English-speaking women living in Paris, the combination of:
means that you have many options to manage adenomyosis and improve quality of life.
If you are experiencing:
it is worth seeking a consultation with a gynecologist experienced in adenomyosis and endometriosis in expat patients. An individualized plan—sometimes combining medication, lifestyle adjustments, and, when needed, procedures such as UAE or hysterectomy—usually offers the best long-term results.

American Hospital of Paris
55 Boulevard du Château,
92200 Neuilly-sur-Seine
+33 (0) 1 46 41 26 99
2025 © Dr Ramírez Zamudio